Substance Abuse and Depression Treatment in New Jersey
The relationship between depression and substance abuse is a two-way street. Often, mental health conditions such as depression can lead to drug and alcohol abuse as a means of coping. On the other hand, substance abuse can put individuals at a higher risk of developing clinical depression.
These co-occurring conditions create a dangerous cycle that can make everyday life difficult, but with the right care approach, individuals can address and learn to effectively manage their health from every aspect and achieve long-term recovery.
At Discovery Institute in New Jersey, our behavioral health treatment center specializes in helping individuals suffering from mental health conditions, such as anxiety, depression, and bipolar disorder, as well as, types of addictions, such as alcohol use disorder (AUD), etc.
How Does Drug Abuse Affect Depression, and Vice Versa?
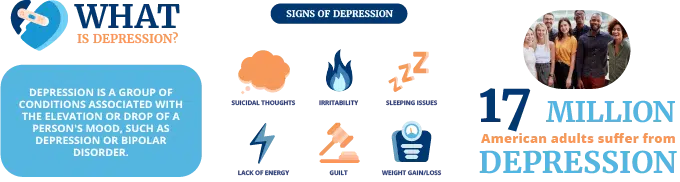
 According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), a major depressive disorder known as depression, is a mood disorder characterized by a persistent feeling of sadness, lethargy, hopelessness, and a lack of interest in everyday life. Depression can be situational and triggered by a specific life event. Or it can be clinical, meaning it occurs for long periods of time with no identifiable source.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), a major depressive disorder known as depression, is a mood disorder characterized by a persistent feeling of sadness, lethargy, hopelessness, and a lack of interest in everyday life. Depression can be situational and triggered by a specific life event. Or it can be clinical, meaning it occurs for long periods of time with no identifiable source.
Many people perceive depression as a “bad mood” or “feeling down,” but depression is much more serious than that. This mental illness occurs when the chemicals and hormones in the brain and body aren’t able to function or regulate properly, ultimately altering the body’s natural chemistry. For this reason, depression should be managed and treated under the supervision of mental health professionals. Depressive symptoms include:
- Mood swings
- Severe sadness, lethargy, irritability, and frustration
- Lack of interest in normal activities and hobbies
- Difficulty thinking, making decisions, and feeling present
- Extreme fatigue
- Insomnia
- Weight fluctuations
- Substance use
- Unexplained body aches and pains
- Recurring thoughts of death or suicide
The Prevalence of Depression and Substance Abuse
Approximately one-third of adults with mood disorders such as depression, also have a drug or alcohol addiction amid a depressive episode, which can last from weeks to months, or even years, the numbing effects of drugs and alcohol seem like an easy solution.
Although the substances may temporarily relieve some of the negative feelings that come with depression, your body will eventually become dependent on them and experience a full-blown addiction with exacerbated depression.
Our bodies are very smart and very adaptable. If we constantly send the message that substances are what will make us feel better, it will adapt to believe that to be true. Where the body once knew how to organically produce “happy” hormones and brain chemicals, it will lose this ability and result in the co-occurrence of depression and substance abuse. The effects of drugs and alcohol will cause further regulation of the body’s chemicals making it much more difficult to control depressive episodes.
Not only does drug abuse intensify common depression symptoms, but it can lead individuals to refuse treatment, thinking that substances are the only solution. People who have a history of drug abuse are at increased risk for developing a mental disorder, and vice versa. People with a history of a depressive disorder, commonly develop dependence and eventually drug addiction. The longer the body functions at this level, the more difficult these conditions will be to treat.
If left untreated, severe health complications can arise, including withdrawal symptoms, which are expected, due to people trying to quit substance use cold turkey. For people with a mood disorder, seeking treatment for substance use and psychiatric illness is a must.
Often these co-occurring conditions last for long periods of time, which is why a licensed mental health professional who understands the complexity of depressive disorders and substance use should be utilized to create an individualized treatment program.
Diagnosing Depression and Substance Use Disorders
 It’s important to see an experienced physician to conduct a full evaluation of your symptoms to receive an accurate diagnosis. When both of these conditions co-occur, treating only one will not make for successful rehabilitation.
It’s important to see an experienced physician to conduct a full evaluation of your symptoms to receive an accurate diagnosis. When both of these conditions co-occur, treating only one will not make for successful rehabilitation.
There are several ways doctors and therapists identify mental health conditions and a substance use disorder (SUD), to, create a treatment plan from the perspective of not one condition, but both simultaneously.
The processes of diagnosing these disorders will likely include the following:
- Physical Examination
- Psychological Examination
- Lab Tests
During these evaluations, the patient will work one-on-one with experienced professionals to understand the severity and specific characteristics of his or her substance addiction and co-occurring depression.
Different types of mental illness and addictions can all fall under the category of similar diagnoses, so it’s important, to be honest with your treatment team about your history of substance use and mental health, thoughts, and experiences that led you to seek help.
CONTACT US
Find out how we can help
Our compassionate counselors are standing by to answer any questions you may have. After helping thousands of people over the last 50 years, we have the resources to help you and your family and all your individual needs.
Why Are Co-Occurring Disorders Difficult to Diagnose?
Comorbidities tend to contribute to one another, making the symptoms more difficult to distinguish. For example, someone with depression may experience more intense substance abuse as a result. At the same time, someone with an intense addiction may develop extreme depression.
What can make the dual diagnosis easier to understand and treat is to determine which illness came first and what led to the evolution of the other. By determining this, doctors are better able to understand the patient’s brain and how it responds to these conditions. Most importantly, they can use the patient’s information from their psychiatric evaluation to identify an accurate diagnosis.
After a diagnosis is made, the detoxification process can begin, and from there, a comprehensive recovery plan designed to specifically address the individual’s experience with the co-occurring conditions will be put in place to simultaneously treat both.
Treating Substance Abuse and Depression
Treatment for a dual diagnosis such as depression and substance abuse will include a blend of mental health services that address both the physical and psychological effects of these conditions. Many factors come into play, and treatment options for mood disorders and substance use typically include a combination of the following:
- Nutritional therapy
- Depression medications
- Meditation and yoga
- Behavioral modification therapy
- Relapse prevention therapy
Antidepressant medications are not always used for treating depression, especially if there is a concern for addiction after substance abuse. However, they have proven successful in a large percentage of patients. Antidepressants including SSRIs and Tricyclics are designed to help the brain’s chemistry function at its normal levels. times they will be prescribed only until the patient has time to readjust.
Individual counseling sessions with a psychiatrist or counselor will be able to address both your mental illness and substance use disorder, and help find the root causes of their co-occurrence. Trauma from past experiences is often a major factor in the development of both conditions and talking with a professional will enable you to learn how to accept and let go of whatever experiences are triggering your depression and addiction.
Holistic approaches should also be integrated into the treatment program for dual diagnosis to teach individuals how to cope with everyday stressors and urges. Yoga and meditation offer tools of relaxation and mindfulness, and acupuncture or massage therapy can lessen the tension that has manifested as a result of chronic stress.
Typically, residential treatment is preferred for patients receiving treatment for a dual diagnosis of depression and substance abuse. Outpatient care is suitable for less severe conditions, but the comorbidity of these conditions calls for a more highly supervised treatment program.
How Long is Treatment?
 The treatment length for major depression and substance use disorders varies from patient to patient but should extend long enough for the individual to fully recover from the substance addiction and stabilize their mental health condition.
The treatment length for major depression and substance use disorders varies from patient to patient but should extend long enough for the individual to fully recover from the substance addiction and stabilize their mental health condition.
The Centers for Disease Control and Prevention (CDC) suggests that the ideal length of time for addiction treatment should include a 30-day inpatient program with an extended program lasting 3-12 months. This is not always an option, whether due to financial reasons or other external circumstances, so patients should stay as long as possible to ensure skills and strategies for coping and staying sober are achieved.
There are many options for substance abuse treatment, including sober living homes, residential treatment programs, intensive outpatient programs (IOP), and outpatient treatment services (OP).
Once your initial treatment is complete, your team of doctors and clinical professionals will be able to advise what the next steps are to successfully address your co-occurring conditions and maintain recovery.
Get Help for Depression and Substance Abuse
Without proper treatment for a dual diagnosis of depression and addiction, these conditions will impact your life negatively and increase in severity. Sobriety and health are achievable, and at the Discovery Institute, we have the experience and knowledge to get you there.
If you or a loved one needs to find the right treatment program to effectively manage co-occurring conditions such as depression and addiction, contact us today to start your journey to a healthy life.
Dr. Joseph Ranieri D.O. earned his BS in Pharmacy at Temple University School of Pharmacy in 1981 and His Doctorate Degree in Osteopathic Medicine at the Philadelphia College of Osteopathic Medicine in 1991. He is Board Certified by the American Board of Family Medicine and a Diplomate of the American Board of Preventive Medicine Addiction Certification. Dr. Ranieri has lectured extensively to physicians, nurses, counselors and laypeople about the Disease of Addiction throughout New Jersey and Pennsylvania since 2012.



